Adult Stem Cell Therapy & Platelet Rich Plasma
Cartilage Injury Damage Repair and Treatment in Sarasota
Click here to view 3-D cartilage repair demonstrations
Often my patients are not quite sure how cartilage damage in their knee, hip or shoulder joint is related to their pain or to arthritis.
Three different types of cartilage exist:
1. Hyaline Cartilage-this is the type found on the ends of all our bones. You may have seen articular cartilage if you have had a chicken “drumstick”-the white cap is articular cartilage. It provides for smooth gliding and a frictionless surface in our joints

2. Elastic Cartilage– found in the ear and nose
3. Fibrous Cartilage– found in the meniscus of the knee and acromioclavicular joint. The menisci are often a source of pain when they tear in the knee. There are two semilunar cartilages in the knee called the medial and lateral meniscus.
The different types have slightly different properties that make each type the most appropriate to fulfill its respective function at that particular site body site.
Cartilage basically consists of two components: water and a framework of a matrix that givess the tissue its form and function. The matrix is highly organized and composed of collagens, proteoglycans and non-collagenous proteins. Simple disruptions in the matrix can often lead to continued breakdown without repair. The interaction of water and the macromolecular framework give the tissue its mechanical properties and thus its function. So when the matrix breaks down, cartilage loses its mechanical function and can’t dissipate the weight properly. Following the underlying bone starts to react and one develops arthritis.
Embedded in this tight matrix are the cells, called chondrocytes. They maintain the matrix. The volume of cells is rather small. In adult human cartilage for example, cells make up about 1-2% of the tissue volume.
Cartilage Damage
Cartilage and the cells called chondrocytes are nourished by diffusion. That means all their nutrients get to the cells from the joint fluid. They get damaged and do not heal well. They have no nerves and no blood supply.
Cartilage is a very organized structure. This makes it particularly difficult to restore or duplicate once it is damaged or lost. Injury to any part of this complex system can disrupt the functional properties of cartilage. In case articular cartilage is involved, this may lead to further joint degeneration.

Dr. Bennett from Sarasota, Florida has been treating cartilage damage for years. Very advanced techniques utilizing stem cells and reprogramming adult chondrocytes can be performed to restore damaged cartilage to normal.

Sarasota Cartilage Repair
Biological Approaches for Cartilage Repair
Musculoskeletal injuries are the most common cause of severe long-term pain and disability. At Bennett Orthopedics and Sportsmedicine, Dr. Bennett, the founder has an armamentarium of approaches to treating your cartilage injury, which range from injections to surgical procedures. The decade from 2000 to 2010 was called the “decade” of bone and joints to launch global awareness and promote further research in the prevention, diagnosis, and treatment of joint injuries.
In the United States, osteoarthritis medicines cost $5.31 billion in 2007, and musculoskeletal conditions including osteoarthritis cost nearly $128 billion per year. Recently the push to maintain and preserve joints has been made with biologic approaches to maintaining, repairing and regenerating joint tissue like cartilage and the underlying bone.
CARTILAGE TREATMENT
All joints in our body have Hyaline cartilage(articular cartilage), which is the “cap” of cartilage on the end of the bone. It combines a smooth surface and the ability to withstand an extreme amount of pressure. Unfortunately, articular cartilage lesions with the inherent limited healing potential, is problematic and the first step to developing arthritis.
Slideshow About Cartilage Treatment
Orthobiological techniques in cartilage lesions are becoming more frequently used. Growth factors and mesenchymal stem cells have been used successfully in many medical fields, such as maxillofacial, cosmetic, spine, orthopedic, and general wound healing applications. Dr. Bennett has utilized these biologic approaches to treat cartilage injuries and arthritis.
CONSERVATIVE TREATMENT AND PREVENTIVE BIOLOGIC SOLUTION
Nonsurgical treatment of cartilage lesions, including diet, intra-articular injections, and rehabilitation were relegated to pain control and activity modifications and do little to restore cartilage anatomy and function. Even lubricating injections, also called viscosupplementation, do little to restore articular cartilage to normal after damage.
Recent studies on pulsed electromagnetic fields and platelet-rich plasma injections and mesenchymal stem cell injections have shown that these methods have the capacity to help heal cartilage tissue and delay osteoarthritis.
Simple weight-loss and cessation of nicotine use have been shown to decrease pain, increase mobility and move a patient to a higher quality of life.
Electromagnetic fields provide chondroprotective treatment for patients immediately following arthroscopic surgery without any negative side effects and it exerts a short-term effect in reducing functional recovery time.
Platelet-rich plasma preparations have been used with effective results both in surgical and outpatient procedures in the treatment of musculoskeletal problems and can be simply injections or used in conjunction with surgical procedure. Dr. Bennett has had great success with both approaches. Simple injections of PRP has been shown to greatly reduce pain and has also been shown in the lab to help cartilage repair. Dr. Bennett uses PRP with ACL reconstruction, meniscal repair and even cartilage microfracture treatment.
PRP
This is a concentration of platelets from your own blood which has many important bioactive proteins and growth factors, such as platelet-derived growth factor, insulin like growth factor, transforming growth factor, epidermal growth factor, fibroblast growth factor, and vascular endothelial growth factor. These factors, when secreted by platelets arriving at an injury site, regulate key processes involved in tissue repair, including cell proliferation, chemotaxis, migration, cellular differentiation, and extracellular matrix synthesis. They recruit stem cells, stimulate stem cells to differentiate, and stimulate adult cells to perform their function.
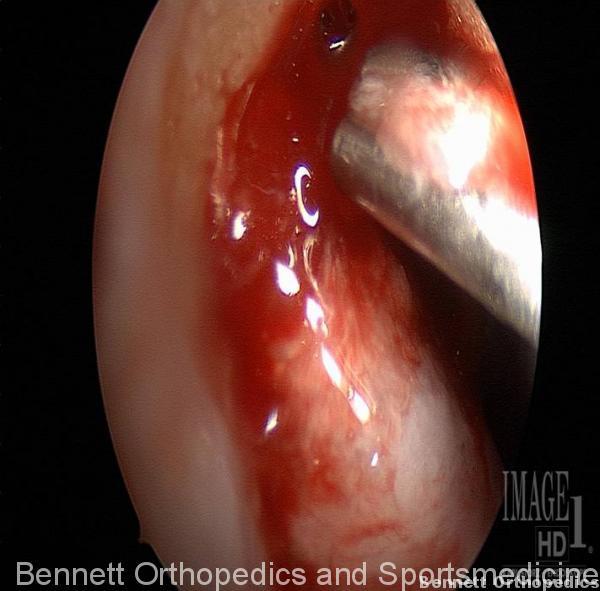
Cartilage Surgical Treatment
Traditional palliative or reparative treatment techniques have demonstrated variable results. The most common cartilage treatment is a meniscal resection: the second a lavage and debridement of articular cartilage. The following procedures in the order that they are discussed progress from the least invasive and shortest rehabilitation time- most of these creating little cartilage repair or cartilage of inferior quality- to those that are more involved and require longer rehabilitation times-these being the procedures that create near normal cartilage.
Lavage and Debridement-Chondroplasty
A chondroplasty can provide symptomatic pain relief with no actual hyaline tissue formation. However, these techniques remove superficial cartilage layers that include collagen fibers responsible for the tensile strength, which creates a functionally inferior cartilage tissue.
Microfracture-Bone marrow Stimulation Techniques

Bone marrow stimulation techniques, such as subchondral plate drilling or microfracture, have been reported to stimulate production of hyaline-like tissue, but in fact create an inferior cartilage called fibrocartilage. Many athletes enjoy this approach because when they are in their down season, realize some cartilage healing. However, with time, this cartilage then wears out again. Thisusually lasts 4-5 years.
Cartilage Transfer Techniques
These are cartilage pug techniques whereby a dowel of cartilage if transferred from within a site inside the knee joint in an area where it is not needed and then placed tightly into an area where there is damaged cartilage. This is usually relegated to areas of 1.5cm or less.
Cartilage Growing Techniques-Carticel
First Generation Cartilage Implantation-Autologous Chondrocyte Implantation (ACI)
This technique and subsequent generational improvements create near normal articular cartilage. The initial technique included a 2 step surgical procedure. The first is a biopsy of adult cartilage from inside the knee. The cells are then grown and sent to a lab where they are deprogrammed and become like a stem cell. They are then grown and multiplied till around 12,000,000 cells. The second procedure required open surgery and the harvesting of a periosteal patch from the patient. With evolving techniques, Dr. Bennett is now performing some of these techniques with an arthroscope. The periosteal patch was implicated in overgrowth and scarring, requiring multiple surgical procedures.
Second Generation Implantation
Dr. Bennett has been performing second generation cartilage implantation for over 6 years. This includes using a scaffold to place the cells behind other than the periosteal patch. He has been using a collagen membrane. Other scaffolds include resorbable polymers and hyaluronic acid derivatives. This allows for a smaller incision and allows for a diminished number of multiple secondary procedures due to adhesions and overgrowth of the periosteal patch.
Third-Generation Autologous Chondrocyte Implantation
Cell specific expansion techniques, arthroscopic approaches, growing cells in a 3-dimensional construct, subjecting the cells in the growth medium to mechanical forces, seeding the cells on the membrane all constitute evolving and new generations of cartilage repair techniques.
Stem Cells
But wait-toward a 1-Step Surgical procedure includes harvesting at the time of surgery bone marrow derived mesenchymal stem cells and placing them into the cartilage defect at the time of surgery. Dr.Bennett has been using these stem cells for 6 years, come to Bennett Orthopedics and Sportsmedicine and get the state-of-art cartilage treatment approaches.

Dr. Bennett’s immediate services area is localized to Sarasota, Bradenton, Venice, North Port, Englewood and Lakewood Ranch. With easy access to Tampa-St. Petersburg Airports, as wellas Ft Meyers airport, his reach extends to Naples, Port Charlotte, out-of-state and International patients.
For more about cartilage repair, surgery and treatment…
Cartilage Regeneration Slideshow






